SPINE CONDITIONS
Disc Prolapse and Lumbar Radiculopathy
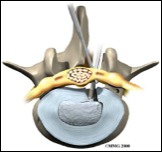
The discs lie between the end surfaces of the vertebrae. They have a strong outer ring and a less strong inner filling. When the water content of the disc decreases, occasionally the outer ring tears and the inner filling spills out through the tear, which can compress the nearby nerve. Symptoms are leg pain, pins and needles in the foot and sometimes weakness and difficulty in passing urine. Disc rupture can be caused by trauma, the normal degenerative ageing process, or both.
Diagnosis is made based on clinical symptoms, clinical examination and is confirmed by CT and MRI scans of the lumbar spine.
80% of patients with disc prolapse will improve with conservative (non-surgical) treatment in the form of analgesics, physiotherapy, perineural cortisone injections and time.
Surgery to remove the protruded fragment is indicated in the following circumstances:
• the presence of cauda equina compression (urinary retention and numbness in the genital area and around the anus)
• large disc fragment with weakness and numbness
• persistence of symptoms after 6 weeks of conservative treatment
The operation is called a "Microdisectomy" and is done through a small incision under microscope magnification. You will be able to walk the same day and will be discharged from hospital 1-2 days after surgery. The surgery carries a very small risk of complications including nerve injury, spinal fluid leak, infection and recurrence. The risk is minimal and your surgeon will explain the risks in detail. The operation has an 80-90% chance of relieving the sciatica component (the pain and the sensory symptoms in the leg) but may have no effect on the back pain - which usually improves with time.
In the first few months after surgery you should avoid lifting objects heavier than 5kg and avoid bending forward. Your surgeon will monitor your progress after surgery and will accordingly advise you to increase your activities over time.
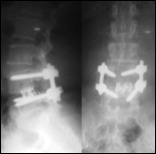
A small proportion of patients who develop recurrent disc prolapses at the same level or recurrent symptoms due to scarring that does not resolve with conservative measures or instability may require fusion of the affected segment (the two adjacent vertebrae) using screws inserted through the posterior part of the vertebra (pedicle) into the vertebral body and bone graft.
Diagnosis is made based on clinical symptoms, clinical examination and is confirmed by CT and MRI scans of the lumbar spine.
80% of patients with disc prolapse will improve with conservative (non-surgical) treatment in the form of analgesics, physiotherapy, perineural cortisone injections and time.
Surgery to remove the protruded fragment is indicated in the following circumstances:
• the presence of cauda equina compression (urinary retention and numbness in the genital area and around the anus)
• large disc fragment with weakness and numbness
• persistence of symptoms after 6 weeks of conservative treatment
The operation is called a "Microdisectomy" and is done through a small incision under microscope magnification. You will be able to walk the same day and will be discharged from hospital 1-2 days after surgery. The surgery carries a very small risk of complications including nerve injury, spinal fluid leak, infection and recurrence. The risk is minimal and your surgeon will explain the risks in detail. The operation has an 80-90% chance of relieving the sciatica component (the pain and the sensory symptoms in the leg) but may have no effect on the back pain - which usually improves with time.
In the first few months after surgery you should avoid lifting objects heavier than 5kg and avoid bending forward. Your surgeon will monitor your progress after surgery and will accordingly advise you to increase your activities over time.
A small proportion of patients who develop recurrent disc prolapses at the same level or recurrent symptoms due to scarring that does not resolve with conservative measures or instability may require fusion of the affected segment (the two adjacent vertebrae) using screws inserted through the posterior part of the vertebra (pedicle) into the vertebral body and bone graft.
Lumbar Spinal Stenosis
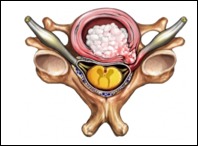
Lumbar spinal stenosis is a narrowing of the lumbar spinal canal, which carries the nerves to the legs. As the spinal canal narrows, the spinal cord and nerves are compressed. Lumbar spinal stenosis results in lower back pain, heaviness and numbness in the legs after walking short distances, and in advanced cases difficulty in passing urine and numbness in the genital and perianal region.
Diagnosis is made based on clinical symptoms, clinical examination and confirmed by an MRI scan of the lumbar spine and occasionally a CT myelogram (injection of contrast material into the lumbar spine via lumbar puncture).
Diagnosis is made based on clinical symptoms, clinical examination and confirmed by an MRI scan of the lumbar spine and occasionally a CT myelogram (injection of contrast material into the lumbar spine via lumbar puncture).
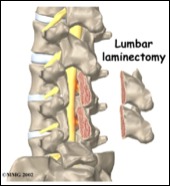
The majority of patients with this condition require spinal decompression, which is called a Laminectomy. The operation involves removing portions of the involved vertebrae and thickened ligaments to create more space. The operation has an 80% chance of improving the leg symptoms and the walking tolerance. There is a small risk of complications which include nerve injury, spinal fluid leak, infection and recurrence. The risk is minimal and your surgeon will explain these risks in detail.
You will be able to walk the same day of the operation and will be discharged from hospital within 2-3 days. If your progress is slow you may need to be referred for rehabilitation. You will have some back pain and stiffness after the operation, which will improve gradually. You will need to see your family doctor one week after the operation to make sure that the wound is OK and you will need to see your surgeon in four weeks time - or sooner if you have any concerns.
You will be able to walk the same day of the operation and will be discharged from hospital within 2-3 days. If your progress is slow you may need to be referred for rehabilitation. You will have some back pain and stiffness after the operation, which will improve gradually. You will need to see your family doctor one week after the operation to make sure that the wound is OK and you will need to see your surgeon in four weeks time - or sooner if you have any concerns.
Cervical Radiculopathy
Cervical radiculopathy is caused by compression of one or more of the nerves to the upper limbs by a disc protrusion or new bone formation. The pain goes to the upper limb and is occasionally associated with pins and needles, numbness in the arm, forearm or hand, and occasional weakness of part of the limb. The pain is sometimes associated with symptoms of compression of the spinal cord, such as clumsy hands, deterioration of gait and electric shock-like feelings in the whole body on sudden neck movement.
Diagnosis is made based on clinical symptoms, clinical examination and a cervical spine MRI scan, CT scan, or both.
Initial treatment is conservative (non-surgical), in the form of analgesics, physiotherapy and cortisone injections. 80% of patients improve with this treatment.
Surgical decompression of the involved nerve is indicated if your symptoms don't resolve after 6 weeks of conservative treatment or if you have weakness or clinical evidence of spinal cord compression. The nerve can be decompressed through two approaches (posterior and anterior), the choice depends on whether there is associated spinal cord compression. Your surgeon will discuss the pros and cons of each approach with you.
You will be able to walk on the day of surgery. Most patients will be discharged the next day.
If the operation is done from the posterior approach (foraminotomy), you will experience muscular neck pain and stiffness which will last 2-3 weeks. The risks of the operation are minimal and include nerve root injury, infection, haemorrhage and and recurrence. The operation has an 80% chance of resolving the arm pain. If the operation is done from the front (anterior cervical disectomy and fusion), neck pain will be minimal if any. The risks of the operation are minimal and include nerve root injury, spinal cord injury, infection, haemorrhage, hoarse voice, swallowing difficulties and potential risk of developing accelerated degenerative changes in the disc above and below the fusion. Your surgeon will explain to you the nature of the procedure and the possible complications in detail.
Diagnosis is made based on clinical symptoms, clinical examination and a cervical spine MRI scan, CT scan, or both.
Initial treatment is conservative (non-surgical), in the form of analgesics, physiotherapy and cortisone injections. 80% of patients improve with this treatment.
Surgical decompression of the involved nerve is indicated if your symptoms don't resolve after 6 weeks of conservative treatment or if you have weakness or clinical evidence of spinal cord compression. The nerve can be decompressed through two approaches (posterior and anterior), the choice depends on whether there is associated spinal cord compression. Your surgeon will discuss the pros and cons of each approach with you.
You will be able to walk on the day of surgery. Most patients will be discharged the next day.
If the operation is done from the posterior approach (foraminotomy), you will experience muscular neck pain and stiffness which will last 2-3 weeks. The risks of the operation are minimal and include nerve root injury, infection, haemorrhage and and recurrence. The operation has an 80% chance of resolving the arm pain. If the operation is done from the front (anterior cervical disectomy and fusion), neck pain will be minimal if any. The risks of the operation are minimal and include nerve root injury, spinal cord injury, infection, haemorrhage, hoarse voice, swallowing difficulties and potential risk of developing accelerated degenerative changes in the disc above and below the fusion. Your surgeon will explain to you the nature of the procedure and the possible complications in detail.
Cervical Myelopathy and Cervical Laminectomy with or without stabilisation
Cervical myelopathy results from compression of the cervical cord. The most common cause is degenerative spine disease. The compression can be secondary to a central disc prolapse, cervical stenosis from a combination of disc prolapse and thickening of the ligaments connecting the bones in the neck (cervical vertebrae). These degenerative changes are occasionally associated with changes in the normal alignment of the vertebrae.
Symptoms are deterioration of gait, clumsiness of hands, pins and needles, or numbness in the upper - and less likely - lower limbs.
Diagnosis is made based on the clinical symptoms, the clinical examination and is confirmed by an MRI scan of the cervical spine. Occasionally you may need to have CT scan and flexion extension films of your spine to assess the bony structures and stability.
The treatment of cervical myelopathy is surgical decompression of the spinal cord through either the front or the back of the neck. Stabilisation of the cervical spine using lateral mass screws from the back or cages and plates from the front may be required. Your surgeon will discuss the surgical options and the pros and cons of each option with you.
It should be understood that the goal of surgery is to prevent further deterioration of spinal cord function. Although the majority of patients improve to some extent after surgical decompression some do not. The surgery should be performed at the earliest convenient time as any loss of function can be permanent.
Symptoms are deterioration of gait, clumsiness of hands, pins and needles, or numbness in the upper - and less likely - lower limbs.
Diagnosis is made based on the clinical symptoms, the clinical examination and is confirmed by an MRI scan of the cervical spine. Occasionally you may need to have CT scan and flexion extension films of your spine to assess the bony structures and stability.
The treatment of cervical myelopathy is surgical decompression of the spinal cord through either the front or the back of the neck. Stabilisation of the cervical spine using lateral mass screws from the back or cages and plates from the front may be required. Your surgeon will discuss the surgical options and the pros and cons of each option with you.
It should be understood that the goal of surgery is to prevent further deterioration of spinal cord function. Although the majority of patients improve to some extent after surgical decompression some do not. The surgery should be performed at the earliest convenient time as any loss of function can be permanent.
Lumbar Spondylolisthesis
Lumbar Spondylolisthesis is the slip of one vertebra over another. The two most common types are Degenerative and Isthmic.
The symptoms are chronic lower back pain and occasional symptoms of nerve compression (pain and pins and needles or numbness in part of the leg or foot).
Diagnosis is made based on the clinical symptoms, clinical examination and radiological studies including the CT, MRI and flexion/extension films of the lumbar spine.
The symptoms are chronic lower back pain and occasional symptoms of nerve compression (pain and pins and needles or numbness in part of the leg or foot).
Diagnosis is made based on the clinical symptoms, clinical examination and radiological studies including the CT, MRI and flexion/extension films of the lumbar spine.
There are four grades of Spondylolisthesis, based on the degree of slip and varying treatments for each:
Your surgeon will discuss the nature of surgery and associated risks with you.
- Grade 1 (less than 25% slip). The initial treatment consists of analgesics, physiotherapy and core stabilising exercises. Surgical fusion is indicated if symptoms are intolerable and are accompanied by severe leg symptoms.
- Grade 2 (25%-50% slip). The majority require surgical decompression and stabilisation.
- Grade 3 (50%-75% slip). The majority require surgical decompression and stabilisation.
- Grade 4 (greater than 75% slip). The majority require surgical decompression and stabilisation.
Your surgeon will discuss the nature of surgery and associated risks with you.
ALWAYS OBTAIN AN OPINION FROM YOUR TREATING DOCTOR ABOUT ANY MEDICAL CONDITION